Introduction: Ischemia is a common consequence of peripheral vascular disease, which affects more than 27 million patients in the United States[1]. Currently, surgical therapies exist for treatment of ischemia, but these treatments are prone to failure in the long term. Regenerative therapies that stimulate the growth of new vasculature have great potential for treating peripheral and myocardial ischemia. Growth factor based therapies that induce neovascularization have been successful in healthy animal models, but have limited success in clinical trials due. This discrepency may be linked to growth factor resistance associated with diseases that lead to peripheral vascular disease[2]. Here, we have developed a new method for enhancing the activity of growth factors in growth factor resistant disease states such as diabetes and hyperlipidemia. Our novel method delivers the growth factor co-receptor glypican-1 embedded in a liposomal carrier to create a glypican-1 proteoliposome (“glypisome”).
Materials and Methods: Liposomes were prepared by resuspending a dried lipid film in HEPES buffer and extruding it through a 400 nm polycarbonate filter. Purified glypican-1 (48.8 µg/ml) was added to the liposome solution to create the glypisomes. Ischemia was induced in the hind limb of mice by ligating the femoral artery. The treatment was delivered by implanted alginate beads (FGF-2, glypisomes, or FGF-2 and glypisomes). Recovery of perfusion in the ischemic hind limb was monitored over 14 days using laser speckle. On day 14, the animals were sacrificed and the thigh and calf muscle tissue was isolated and process for paraffin sections. The sections were immunostained for PECAM to quantify neovascularization.
Results and Discussion:
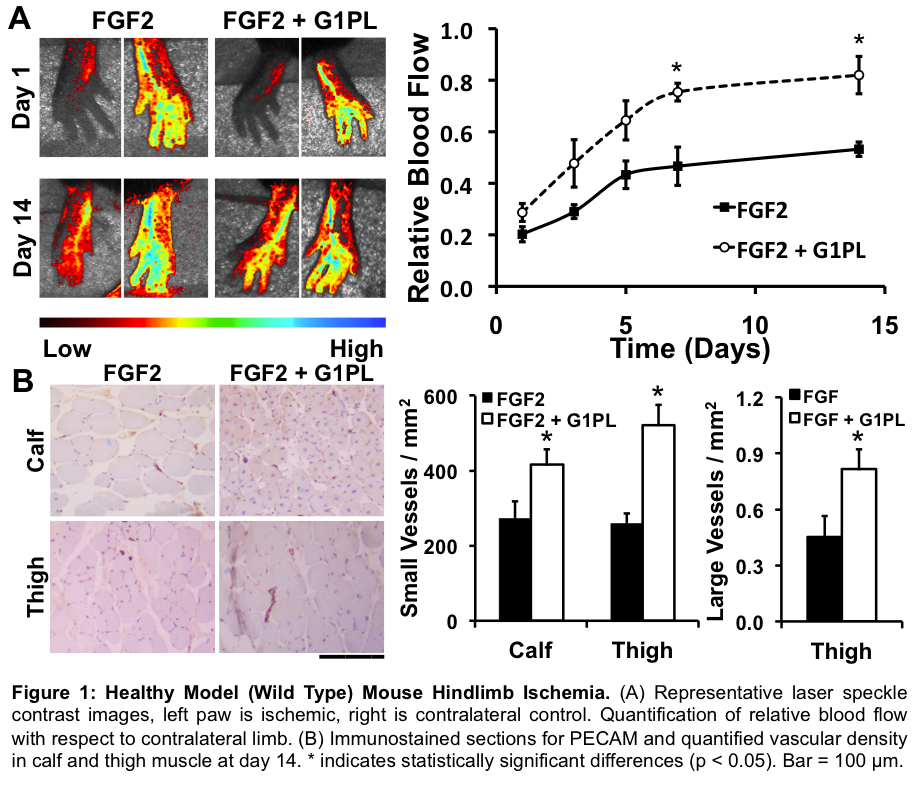
In our healthy animal model we saw an increase of angiogenic response to FGF-2. Wild type mice treated with FGF-2 and glypisomes exhibited a significant increase in relative blood flow 7 and 14 days post injury (Figure 1A). Co-delivery of FGF-2 and glypisomes also led to a significant increase in small vessels in both the calf and thigh compared to FGF-2 alone, as well as a significant increase in large vessel density in the thigh muscle of mice (Figure 1B).
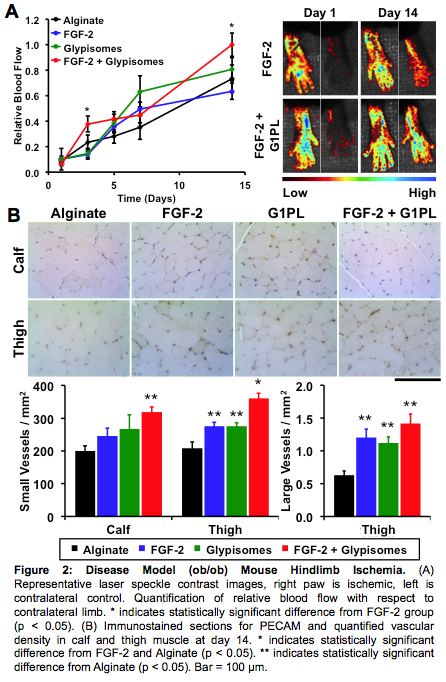
For our disease model we used ob/ob mice, these mice are leptin deficient, obese and hyperlipidemic and are used as a model for diabetes. Ob/ob mice treated with FGF-2 and glypisomes exhibited a significant increase in relative blood flow compared to mice treated with just FGF-2 alone 3 and 14 days post injury (Figure 2A). Co-delivery of FGF-2 and glypisomes also led to a significant increase in small vessels in calf and large vessels in the thigh muscle compared to the alginate control (Figure 2B). Co-delivery of FGF-2 and glypisomes led to a significant increase in small vessels in the thigh when compared to FGF-2 alone (Figure 2B).
Conclusion: Glypisomes delivered in combination with FGF-2 from an alginate gel increases revascularization of ischemic hind limb in both wild type and disease model mice. We see not only an increase in recovered blood flow relative to the contralateral control, but also an increase in overall vascular density in the thigh and calf muscle at 14 days post injury. Thus, locally delivered growth factors in combination glypisomes may be a promising approach for treating peripheral vascular disease and overcoming growth factor resistance.
NIH; American Heart Association; The Welch Foundation
References:
[1] O'Donnell ME, et al Ulster Med J 2011. 80(1): pp 33-41
[2] Das S, et al, Biomaterials 2014. 35(1): pp 196-205