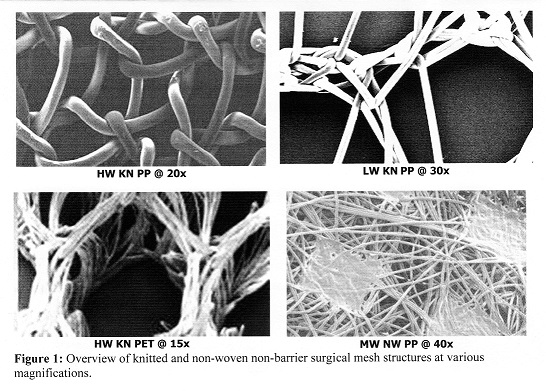
Synthetic surgical mesh has become an important tool in the armamentarium of the surgeon reconstructing soft tissue defects and hernias. Mechanical failure and recurrence remain primary causes of repair revision and mesh removal in hernia repair[5]-[30]. This study evaluated the qualitative and quantitative morphology of intramesh fibrous connective tissue (FCT) healing in a range of clinically used knitted (polypropylene and polyester) and non-woven (polypropylene) barrier and non-barrier surgical meshes implanted in a rabbit model.
The results demonstrated that the knitted mesh displayed intramesh FCT healing that was concentric to the mesh fibers[27] with significant between fiber FCT discontinuities due to the presence of adipose tissue. Non-woven surgical mesh resulted in a more linearly oriented intramesh FCT healing, primarily parallel to the plane of the non-woven mesh, with minimal FCT discontinuity.
Non-woven surgical mesh had a significantly reduced incidence of FCT discontinuity and a higher probability of a FCT response than knitted surgical mesh.
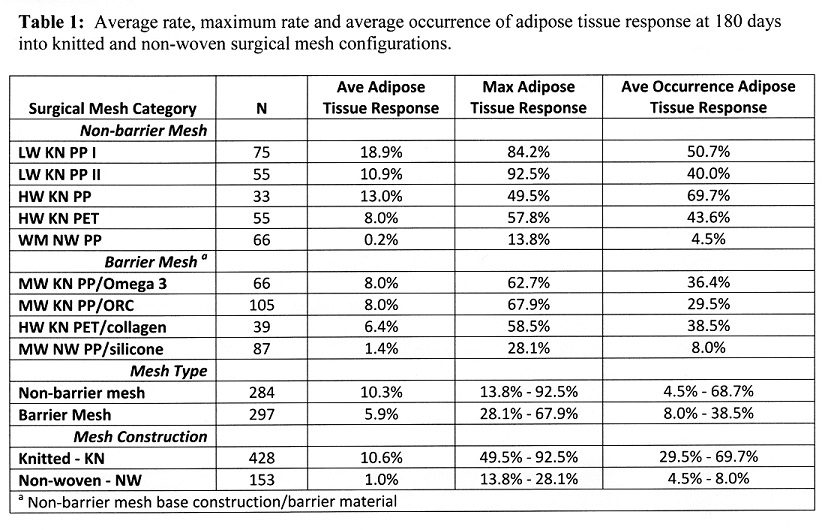
The presence of significant discontinuities in intramesh FCT healing in this study, especially in lightweight knitted surgical mesh which has been associated with mechanical failures clinically[16],[17], underscores the importance of complete FCT healing for secure long term hernia repair. In conclusion, non-woven monofilament constructions of barrier and non-barrier surgical mesh resulted in highly congruent intramesh FCT healing when compared to commonly used barrier and non-barrier knitted surgical mesh constructions which demonstrated significant FCT healing discontinuities.
BG Medical; Dartmouth Hitchcock Surgical Research Lab
References:
[1] Flum DR, Horvath K, Koepsell. Have outcomes of incisional hernia repair improved with time? Ann Surg 2003; 23: 129-135
[2] Vrijland WW, van den Tol MP, Luijendink RW, Hop WC, Busschbach JJ, de Lange DC, van Geldere D, Rottier AB, Vegt PA, Ijzemans JN, Jeekel J. Randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. BJS 2002; 89: 293-297
[3] Luijendijk RW, A comparison of suture repair with mesh repair for incisional hernia. New Engl J Med 2000; 343: 392-39
[4] Heniford BT,Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 2003; 238: 391-400
[5] Klosterhalfen B, Junge K, Klinge U. The lightweight and large porous mesh concept for hernia repair, Expert Rev. Med. Devices 2005; 2: 103-117
[6] Robinson TN, Clarke JH, Schoen J, Walsh MD. Major mesh-related complications following hernia repair. Surg Endosc 2005; 19: 1556-1560
[7] Binnebosel M, Klink CD, Otto J, Conze J, Jansen PL, Anurov M, Schumpelick V, Junge K. Impact of mesh positioning on foreign body reaction and collagenous ingrowth in a rabbit model of open incisional hernia repair, Hernia 2010; 14: 71-77
[8] Raptis DA, Vichova B, Breza J, Skipworth J. Barker S. A comparison of woven versus nonwoven polypropylene (PP) and expanded versus condensed polytetrafluoroethylene (PTFE) on their intraperitoneal incorporation and adhesion formation, J Surg Res 2011; 169: 1-6
[9] Cobb WS, Burns JM, Peindi RD, Carbonell AM, Matthews BD, Kercher KW, Heniford BT. Textile analysis of heavy weight, mid-weight and light weight polypropylene mesh in a porcine ventral hernia model, J Surg Res 2006; 136: 1-7
[10] Deeken C, Abdo MS, Frisella MM, Matthews BD. Physicomechanical evaluation of polypropylene, polyester and polytetrafluoroethylene meshes for inguinal hernia repair, J Am Coll Surg 2011; 121: 68-79
[11] Cobb WS, Kercher KW, Heniford BT. The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 2005; 12: 63-69
[12] Bury K, Smietanski M.Five-year results of a randomized clinical trial comparing a polypropylene mesh with a poliglecaprone and polypropylene composite mesh for inguinal hernioplasty, Hernia 2012; 16: 549-553
[13] Chowbey PK, Garg N, Sharma A, Khullar R, Soni V, Baijai M, Mittal T. Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc 2010; 24: 3073-3079
[14] Khan LR, Liong S, deBeauz AC, Kumar S, Nixon SJ. Lightweight mesh improves functional outcome in laparoscopic totally extra-peritoneal inguinal hernia repair. Hernia 2009; 14: 39-45
[15] Welty G, Klinge U, Klosterhalfen B, Kasperk R, Schumpelick V. Functional impairment and complaints following incisional hernia repair with different polypropylene meshes. Hernia 2001; 5: 142-147
[16] Cobb WS, Central mesh failure with lightweight mesh: a cautionary note. Hernia Supp I 2009; 13: S38.
[17] Lintin LA, Kingsnorth AN, Mechanical failure of a lightweight polypropylene mesh. Hernia 2014; 18: 131-133
[18] Zuvela M, Galun D, Djuric-Stefanovic A, Palibrk I, Petrovic M, Millicevic M. Central rupture and bulging of a low-weight polypropylene mesh following recurrent incisional sublay hernioplasty. Hernia 2014; 18: 135-140
[19] Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V. Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 1998; 164: 951-960
[20] Howard, V. and Reed, M.G., Unbiased Stereology: Three-dimensional Measurement in Microscopy, 2nd Ed., Garland Science, New York, 2005
[21] Baddeley, A. and Vedel Jensen, E.B., Stereology for Statisticians: Monographs on Statistics and Applied Probability 103, Chapman & Hall/CRC, Boca Raton, FL, 2004
[22] Langer C, Neufang T, Kley C, Liersch T, Becker H. Central mesh recurrence after incisional hernia repair with Marlex – are the meshes strong enough? 2001; 5: 164-167
[23] Cobb WS, Kercher KW, Heniford BT. The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 2005; 12: 63-69
[24] Kling U, Klosterhalfen B, Kirkenhauer V, Junge K, Conze J, Schumpelick V. Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res 2002; 103: 208-214
[25] Amid PK, Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia 1997; 1: 15-21
[26] Bauer JJ, Salky BA, Gelernt IM, Kreel I. Repair of large abdominal wall defects with expanded polytetrafluoroethylene (PFTE). Ann Surg 1987; 206: 765-769
[27] Bellon JM, Contreras LA, Bujan J, Palomares D., Carrera-San Martin A. Tissue response to propylene meshes used in the repair of abdominal wall defects. Biomaterials 1998; 19: 669-675
[28] Wood AJ, Cozad MJ, Grant DA, Ostdiek AM, Bachmann SL, Grant SA. Materials characterization and histological analysis of explanted polypropylene, PTFE, and PET hernia meshes from an individual patient. J Mater Sci: Mater Med 2013; 24: 1113-1122
[29] Carlson MA, Frantzides CT, Shostrom VK, Laguna LE. Minimally invasive ventral herniorrhaphy: an analysis of 6,266 published cases. Hernia 2008; 12: 9-22
[30] Klosterhalfen B, Klinge U. Retrieval study of 623 human mesh explants made of polypropylene – impact of mesh class and indication for mesh removal on tissue reaction. J Biomed Mater Res B 2013; 101: 1393-1400
[31] Cinti S, Mitchell G, Barbatelli G, Murano I, Ceresi E, Faloia E, Wang S, Fortier M, Greenberg AS, Obin MS. Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J Lipid Res 2005; 46: 2347–55
[32] Fried SK, Bunkin DA, Greenberg AS. Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: depot difference and regulation by glucocorticoid. J Clin Endocrinol Metab 1998; 83: 847–5
[33] Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003; 112: 1796–808
[34] Xu H, Barnes GT, Yang Q, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 2003; 112: 1821–30
[35] Costello CR, Bachman SL, Ramshaw BJ, Grant SA. Materials characterization of explanted polypropylene hernia meshes. J Biomed Mat Res B: Appl Biomater 2007 Oct; 83(1): 44-9